Cancer research funding seems biased against men
Or just biased in particular against prostate cancer
You have no doubt seen headlines like these:
You might also have concluded this might have been true in the past (and maybe not even that) and probably isn't true today. Well, I decided to check after a friend's girlfriend asked. So what do we need?
Some list of diseases, their prevalence and deaths.
A matching list of funding for those diseases.
The male vs. female % of cases/deaths of the diseases.
I decided to look at cancer to keep things fairly similar. There are a lot of cancer types, so possibly this is enough variation that we can use. For prevalence and death counts, I settled on US data from here:
And funding data from here, also US (American Cancer Society):
The lists don't match up perfectly (22 types for funding, 19 for counts). I had GPT match them up, and the matchings seemed sensible enough (n=19). With this in hand, I computed the male % of cases and of deaths. Here's the correlations:
Generally, funding seems relatively sensibly allocated, correlating (funded amount) 0.77 with new cases per year and 0.56 with deaths. The correlations with male % of cases/deaths was -0.33 to -0.40, but p's are around 0.09 to 0.18. Let's have a look at the main primary and see if it makes sense:
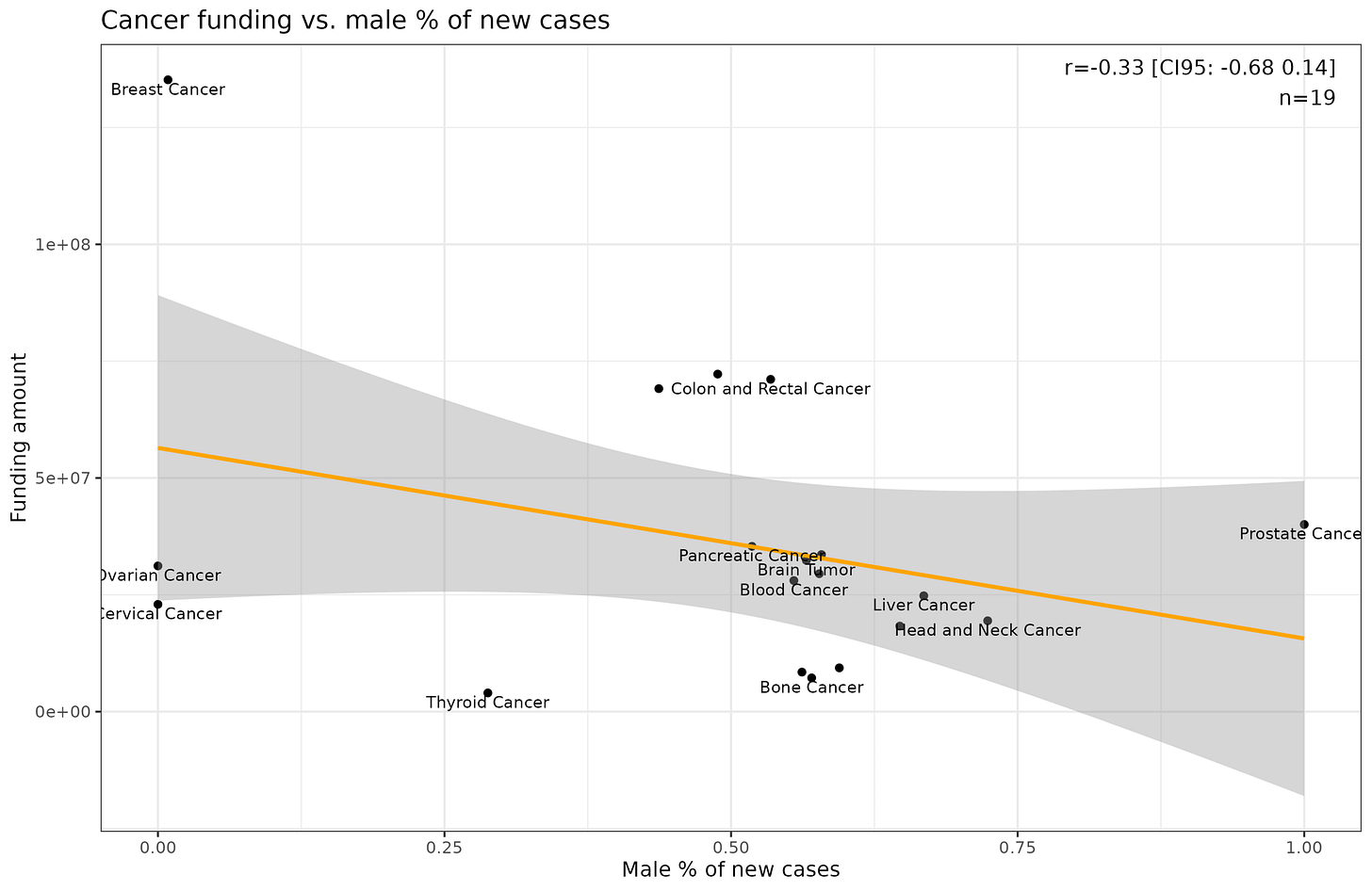
This look sensible enough, and here we can also see where the correlation with male % is from by comparing prostate (100% male) vs. breast (0.9% male). Here's male % vs. funding:
Female cancers appear to be overfunded compared to prevalences, or prostate cancer underfunded. Perhaps the most sensible way to model this is: funding ~ cases_per_year * male_pct_cases. This model yields:
The interaction is p = 0.9% which is impressive considering we only have 19 cases (adjusted r² = 82%). The difference in slope tells us how much funding is allocated per new case a year, by sex. We can plot this to see the effect:
So, female cancers appear to be funded about 3x the ratio of the male ones. We can numerically verify this by computing the male and female implied slopes: 387 / (387-260) = 3.05.
But OK, maybe we need to look at the deaths instead of cases. One could make an argument this is more sensible, since some cancers may be scary and common, but not so dangerous. Alternatively, maybe they are not so dangerous because research into their treatment is well-funded. In any case, this is the model:
The interaction has p of 1.4%, slightly worse, but not bad for this data. The model even predicts that additional male deaths is associated with a decline in funding. The death model fit worse though (adj. r² = 60%), so it is probably wiser to use the cases model.
This is admittedly a rather crude study, but at least insofar as cancers are concerned, it appears there is half-decent evidence that research funding is unfair to men. The 3 female cancers breast, ovarian, cervical get about 135M, 23M, 31M = 189M USD in funding and kill about 70k people/year, thus, 2.7M/1k deaths, while the male cancer prostate gets 40M and kills about 36k/year, or 1.1M/1k deaths. Some of the rarer female cancers were put in the other category and one might want to change this (uterus, vulva) but they are relatively rare anyway (same is true for testis). Given the dataset above, the findings hinge entirely on the prostate cancer datapoint, so it would be wise to get a larger list of diseases.










Part of the problem is that prostate cancer is, often times, the sort of cancer you live with rather than the sort that kills you, no matter what ends up on the death certificate, because a) something else you are also suffering from will get you first and b) by the time you get it you are too old to be a candidate for certain aggressive treatments, and c) the reduced quality of life you can get as a result of the treatments makes many patients decide it is not worth it. But breast and ovarian cancer are mostly diagnosed in otherwise healthy young women, which makes it something you nearly always want to treat.
A couple of considerations:
First, as Laura Creighton noted, the age at which people are impacted is another consideration besides the raw number of deaths. There is data on estimated years of life lost (https://progressreport.cancer.gov/end/life_lost). They estimate in 2022 that breast cancer deaths caused the loss of 710K years of life, ovarian cancer 221K years, corpus & uterus cancer 204K years, cervix uteri cancer 98K years, and prostate cancer 311K years. While breast cancer kills only slightly more people than prostate cancer, it is eliminating over twice as many person-years.
Second, it looks like breast cancer is the main outlier driving much of your results, and this is not surprising to me. In the US, breast cancer awareness is a huge movement that gets lots of attention (https://en.wikipedia.org/wiki/Breast_cancer_awareness). People wear pink ribbons, there's lots of advertising and corporate sponsorship, they even try to tap into sex appeal by selling "I heart boobies" merch. I don't think any other disease has anywhere close to the same PR campaign and lobbying effort. Looking at your results, it doesn't look like there is a strong systematic bias towards funding female cancers in general, mostly just breast cancer in particular, likely as a result of successful campaigning.
When you look at funding per years of life lost by cancer type, you get 0.19 $M/1k yrs for breast cancer, 0.14 $M/1k yrs for ovarian cancer, and 0.13 $M/1k yrs for prostate cancer. Your funding dataset does not mention uterine cancer at all, which is a major killer, so I'm guessing it is merged under the cervical cancer heading, which would yield 0.08 $M/1k yrs (otherwise it would be 0.23 $M/1k yrs for cervical cancer and 0 $M/1k yrs for uterine cancer, which would seem odd). So it looks like breast cancer is a large outlier, whereas prostate cancer is at a similar level of funding to ovarian cancer and well above cervical/uterine cancer.