Explaining HIV's effect on life expectancy in Africa
The magic of antivirals
There's this figure floating on Twitter:
Can anyone explain why insanely HIV rates in southern Africa have absolutely no impact on life expectancy?
Botswana has 10X the rate of HIV as their neighbor Angola, but the average Botswanan lives 5 more years.
Clearly, HIV does not drive the low life expectancy in Africa.
It's an intriguing finding! My initial thoughts were:
The data are wrong, there is nothing to explain.
High frequency of deaths in younger ages before AIDS kills.
High frequency of genetic mutations in those countries that prevent AIDS from killing you.
High rate of antiviral treatments blunts the impact.
First, verifying the results, we can look at HIV prevalence across the world per OWID:
It basically looks like Christian Africa is affected, in particular the southernmost part. Here's life expectancy per OWID:
There doesn't appear to be much relationship. If anything, it might be negative since the lowest life expectancies are in the central area. Here's my reproduction of the initial figure using data for 2019 to avoid any COVID issues:
There is indeed no relationship, so we have something to explain. Of course, one could go full conspiracy mode and claim that HIV doesn't cause AIDS, but let's try the obvious ideas first. We have ruled out (1), so let's check the unstated assumption that HIV causes mortality. Since HIV isn't evenly spread in the world and we don't want other variation to confuse us, it is useful to look just at SSA. Fortunately, someone on Reddit already partially looked at this:
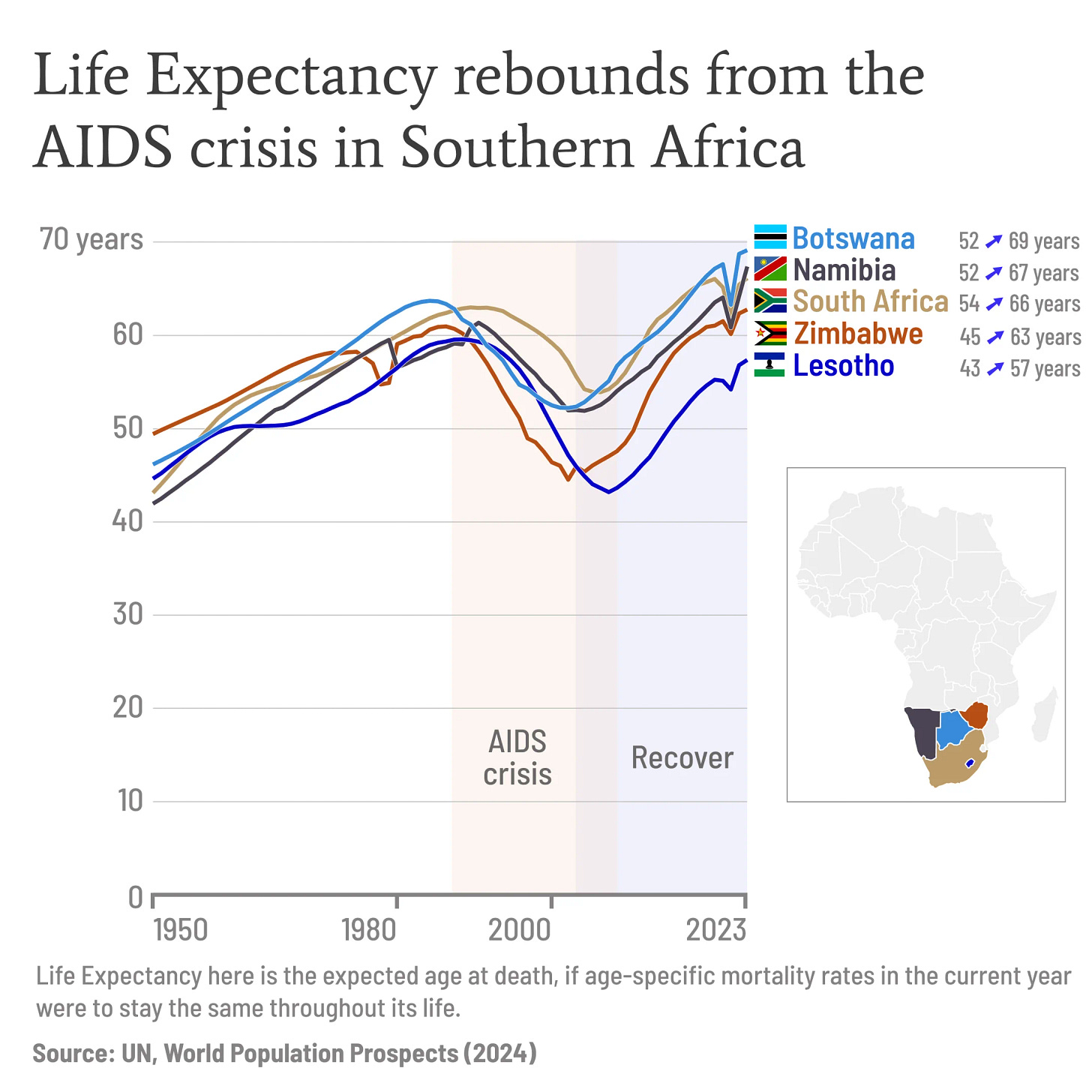
So clearly life expectancies did decrease for a time in the most affected region once HIV started spreading, but then recovered. Better would be to check this formally in comparison with the less-HIV affected African countries. So we can group Africa into two groups based on HIV prevalence and check the average movement of life expectancy:
Individual countries have dubious data and various civil wars and other disasters, but the averages show a very clear pattern where starting in 1988 or so, there is a massive drop in life expectancy in the most HIV affected countries.
We can got one step further. The recovery of life expectancy was because westerners developed antivirals and sold or donated them to Africans. We have data for the proportion of people living with HIV who get treatment. Thus, there should be an interaction such that life expectancy is less affected by HIV% the higher the treatment rate is. Modeling this kind of data the exactly correct way with fixed effects and nonlinear interactions was beyond my immediate knowledge, but I made a linear model and asked Grok to specify the mgcv code for the fancy model. The results for the model predictions were made using the excellent ggeffects package:
This shows the model: life_expectancy ~ year + HIV * HIV_treatment for SSA countries (more complex for the GAMM). The results show a strong interaction such that life expectancy is almost unaffected if the HIV% treatment is 100%. An amazing result! The two models largely agree, but the fancy more is less certain (the confidence intervals overlap a bit). It is also curious that life expectancy is a little higher in regions with more HIV treatment even if HIV is nearly 0%. My interpretation is that treatment % is not random, so the countries which in general do better also have higher coverage even if they only have a tiny number of HIV cases, and thus their life expectancy at ~0% HIV prevalence is a little higher too.
The results are broadly in agreement with studies of individuals. If HIV is constantly treated, mortality is starkly decreased, but it is higher than for other people. Why is that? One study pooled data from 13 datasets:
ART continues to dramatically reduce rates of mortality attributable to HIV-1 infection in high-income countries. Lower rates of deaths due to AIDS after the year 2000 may result from newer ART regimens having better potency and tolerability. However, AIDS remains the most common cause of death, particularly early after initiation of treatment. The strong inverse association of rates of death due to AIDS with CD4 counts at the time of starting ART supports arguments for earlier initiation of ART [31–33]. Conditions associated with social and lifestyle factors contribute the next most frequent causes of death, with violence and liver-related diseases (mainly due to hepatitis) contributing 15% of all deaths. The importance of lifestyle is reinforced by the observation that the most common non-AIDS malignancy reported was lung cancer, likely associated with smoking. Many endocarditis cases occurred in patients infected with HIV-1 via injection drug use, who likely acquired endocarditis through injection drug use. Increases in rates of deaths due to causes associated with aging, such as non-AIDS malignancies and cardiovascular disease, imply that the process of aging will become a dominant factor in HIV-1 mortality in the next decade. Interventions to address risk factors for lifestyle-related causes of death, as well as monitoring for and care of diseases associated with old age, will be necessary if the full benefit of ART in decreasing mortality is to continue in the second decade of ART.
Thus, the problem of comparing HIV-positive treated people vs. controls is that it is far from random who gets HIV in the first place. My speculation for the African results is that this selection bias is much weaker.








Higher life expectancy of some subgroups with HIV is not new (in 2020 I read some numbers in the US). If you get treated, you see medics more often than you might as a non-HIV male (guys are prone to do too little prevention/check ups). Some even might reconsider their lifestyle (smoking, drugs, unprotected intecourse).
In short, hooray for antiviral drugs! And some shame on Trump for killing that program (African countries or the Gates et al. should have taken over long ago, though.).
Are we sure these Africans even have HIV? Remember for reasons of cost an actual HIV test isn't required for a diagnosis in Africa.